A woman’s insulin levels in midlife are linked to the timing and duration of menopausal hot flashes, night sweats and cold sweats, according to new research from the University of Victoria (UVic).
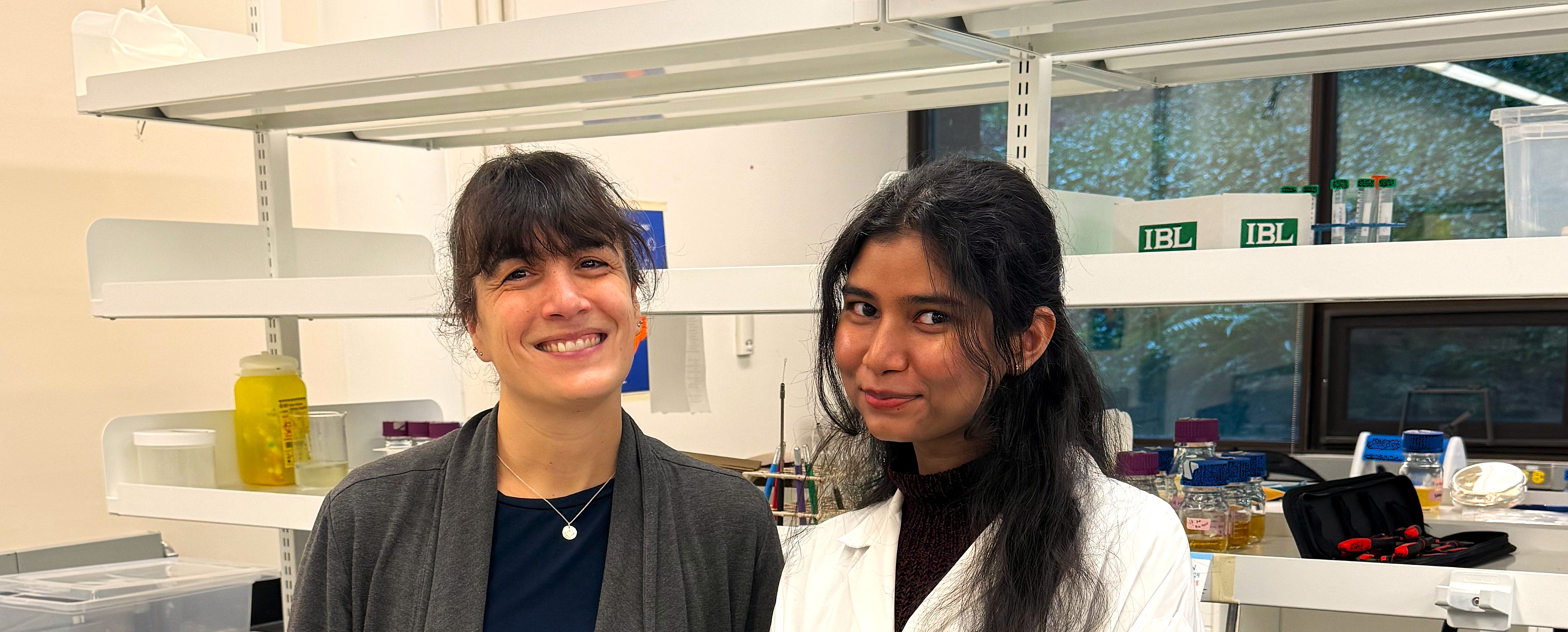
The study found that having higher insulin levels at age 47 predicted younger onsets of hot flashes and night sweats,” says Faria Athar, lead author of the study, which is published in The Journal of Clinical Endocrinology & Metabolism.
“Higher insulin at age 47 was also associated with longer durations of hot flashes and cold sweats, and a rise in testosterone levels across the menopausal transition.
These findings help us to fill some of the gaps in our understanding of menopause symptoms and why their severity varies for different women.”
—Faria Athar, UVic PhD graduate
The burden of vasomotor symptoms
Hot flashes, night sweats and cold sweats—collectively referred to as vasomotor symptoms—affect around 75 per cent of women during the menopausal transition.
These symptoms can appear two years before a woman’s final menstrual period and persist for as long as 10 years beyond it. They dramatically impact women’s quality of life.
It is hard to present at a board meeting while experiencing a sudden sensation of feverish warmth, with a face turning beet red. It is tough to care for elders or children, and to show up for work as a police officer or surgeon, when nightly sleep is disrupted by drenching sweats.
These symptoms do not impact all women equally. Age of onset, severity and duration of vasomotor symptoms vary between women.
Prior research shows factors such as race, ethnicity, and socioeconomic status to play a role. For instance, more Black women report symptoms than women of Asian descent, and the symptoms of women with the same ethnicity may vary depending on where they live and their socioeconomic status.
Menopause and metabolic health
“There’s been a growing awareness of the interplay between metabolic health and reproductive health,” says Nicole Templeman, assistant professor of biology at UVic, and Tier 2 Canada Research Chair in Metabolic Determinants of Reproduction and Aging.
For example, women with higher body fat percentages report more frequent and severe vasomotor symptoms, and particularly early in the menopausal transition. Insulin resistance is also associated with a greater incidence of these symptoms. Finally, increased vasomotor symptom severity has been associated with a higher risk of incidental type 2 diabetes.
“Given that insulin may be elevated in the early stages of metabolic disorders, we decided to investigate whether insulin levels prior to menopause might inform the incidence and severity of menopause symptoms,” says Templeman.
The study and its findings
The research drew upon data from the Study of Women’s Health Across the Nation (SWAN), which followed women longitudinally from a pre-/perimenopausal baseline (42-52 years of age) over 10 years, across seven sites in the United States.
Using metabolic measurements collected from participants at the age of 47, Athar, Templeman, and their coauthors tested how metabolic traits at this early study time point related to physiological features of the menopausal transition.
The researchers observed that insulin levels and body mass index (BMI) at 47 years old were both predictors of vasomotor symptom timing and duration. The most pronounced statistical association for each was a correspondence between higher insulin or BMI and a younger onset of hot flashes.
The analyses showed that insulin may be a stronger predictor of hot flashes when taking other metabolic variables into account, whereas BMI appeared more closely associated with the dynamics of estrogen level changes.
Hope for effective lifestyle interventions
These research findings raise the question of whether women might be able to forestall or manage vasomotor symptoms by lowering their insulin levels—through lifestyle interventions such as a healthy diet and physical exercise.
Reversing obesity is complex and challenging. However, in some cases insulin levels may be more responsive than body composition to lifestyle changes. For instance, exercise training can lower insulin even without concurrent weight loss.
Such possibilities are worth further investigation, as this study indicates that metabolic health—including insulin levels—of women in their 40s might play a role in shaping the experience of the menopausal transition.
Read more about the Templeman Lab here.
This research was supported by funding from the Canadian Institutes of Health Research and Michael Smith Health Research BC.
This research aligns with the United Nations Sustainable Development Goal (SDG) 3 (good health and well-being). Learn more about the SDGs at UVic.